Breathing Filters
Everyday millions of health care professionals dedicate their work to detect and cure disease while caring for their patients. We provide filtration technology which can help to control the contamination and infection risks associated with mechanical ventilation and other medical gases.


Problems
Anesthesia cross-contamination and cross-infection
The Problem
If patients are not provided with a clean anesthesia workstation, there is a high risk of cross-contamination and cross-infection. Studies have shown that the contamination rate of the anesthesia breathing system and circle system amounted to 8–13%.1
Download infographic “Routes of Contamination”
The Solution
The anesthesia breathing circuit needs to be kept clean for every patient. There are two main options:
1. Provide every patient with a new or a clean reprocessed breathing circuit and clean certain parts of the ventilator after the procedure.
2. To use a new high efficiency hydrophobic filter for every patient, which will keep the lumen of the breathing circuit free of patient-derived contamination and enables the use of the same circuit between patients, reducing time and cost and improving efficiency and to perform surface disinfection.
Download flyer "Multiple-Patient-Use-Anaesthesia Circuits"
The Proof
The problem of infection via the anesthesia workstation was identified in the 1960’s and 70’s, with sporadic occurrences also later.2,3
The use of a high efficiency hydrophobic breathing circuit filter (Ultipor 25) has been shown in clinical studies to prevent the spread of patient-derived contamination into the breathing system and allowed for the extended use of filter-protected breathing systems. Cost for disposable products, logistics and waste was reduced by over 40% after using the breathing circuit between all patients on a list for 24h and changing the filter on every patient.4,5
Read our blog "Greening the operating room"
Products
The safety of patients and healthcare workers is our top priority. To prevent bacterial or viral contamination between patients and breathing systems, we’ve designed a range of high efficiency ventilation and breathing system filters. Get quality filters for anesthesia, intensive care and surgical gas handling.
References
Kramer A. et al. (2010). Infection prevention during anaesthesia ventilation by the use of breathing system filters (BSF): Joint recommendation by German Society of Hospital Hygiene (DGKH) and German Society for Anaesthesiology and Intensive Care (DGAI). GMS Krankenhhyg Interdiszip; 21: 5(2)

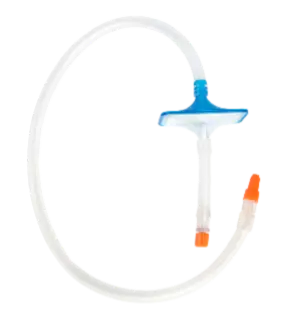
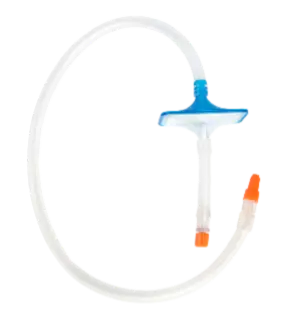
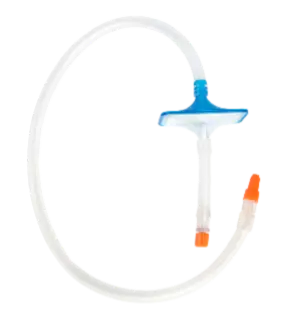
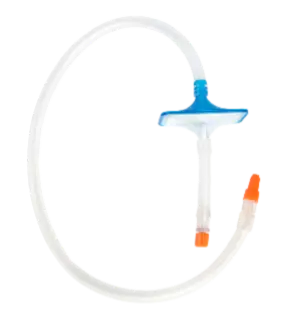
Anaesthesia patient side
Our UltiporTM 25 Breathing Circuit Filter for anesthesia with high efficiency pleated hydrophobic membrane, provides an effective barrier against viruses, bacteria, and liquid-borne contaminants.

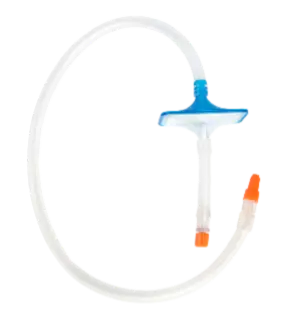
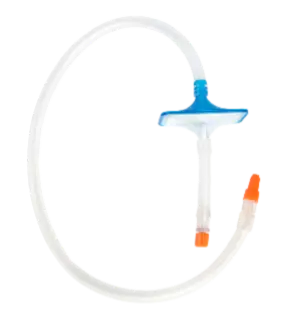
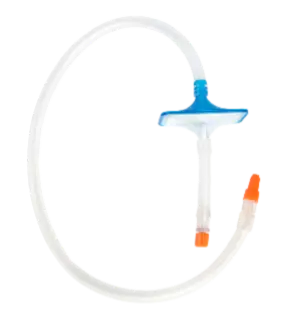
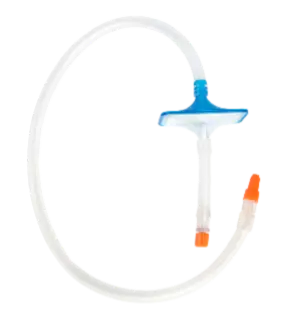
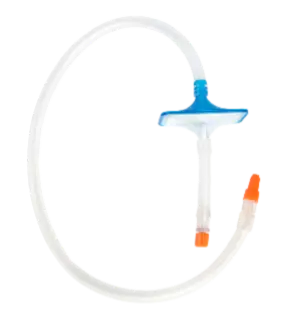
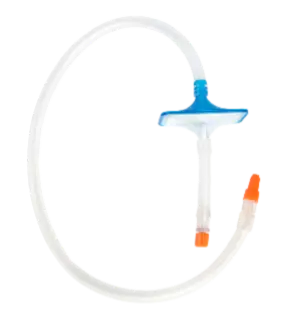
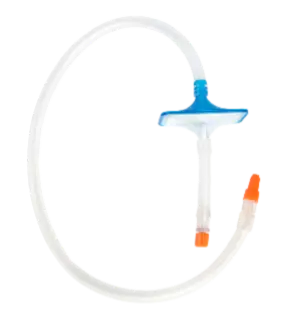
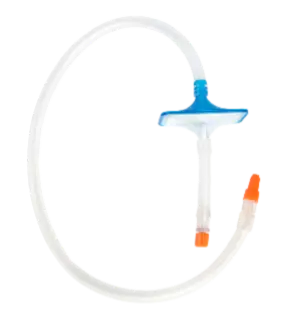
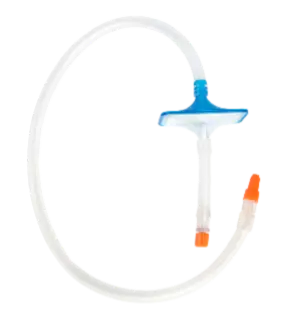
Anaesthesia circuits and kits
(Only available with FDA clearance)
Our multi-patient-use breathing circuits can be used between patients for up to 24 hours if every patient is provided with a new Pall UltiporTM 25 breathing circuit filter. This set up is protecting patients, staff, and equipment while increasing efficiency and reducing costs.

Anesthesia and ICU patient side
Our UlitporTM 100 Breathing Circuit Ffilter with high efficiency pleated hydrophobic membrane, provides an effective barrier against viruses, bacteria and liquid-borne contaminants, and ensures physiological humidification of breathing gases. It can also be used for drug nebulization between the filter and the patient.
If no nebulization is used, the service life of UltiporTM 100 can be extended from 24 to 48 hours.

Machine and patient side anesthesia
Our UltiporTM 50 & 55 Breathing Circuit Filter with highly efficient pleated hydrophobic filter medium is designed for ventilator machine side applications and provides an effective barrier for viruses, bacteria, and liquid-borne contaminant. It can also be used as a heat and moisture exchanger filter at patient end in anaesthesia applications.

Highly efficient surgical smoke evacuation
Our LaparoShield® Laparoscopic Smoke Filtration System with ULPA filtration rating and Viral and Bacterial retention, delivers protection for healthcare workers and patients exposed to surgical plume. It is easy to use and works without the need for external pumping equipment.
Insufflation Gas Filtration
Protect your equipment with our IGF1 Insufflator Gas Line Filter (CE Mark) high efficiency hydrophobic filter medium, protecting against microorganism, particles and backflow of bodily fluids and blood.
The products advertised within this website may not have been licensed in accordance with local regulatory laws. Please check with the local Pall office for availability.
Liquid-borne Bacterial and Viral cross-infection
The Problem
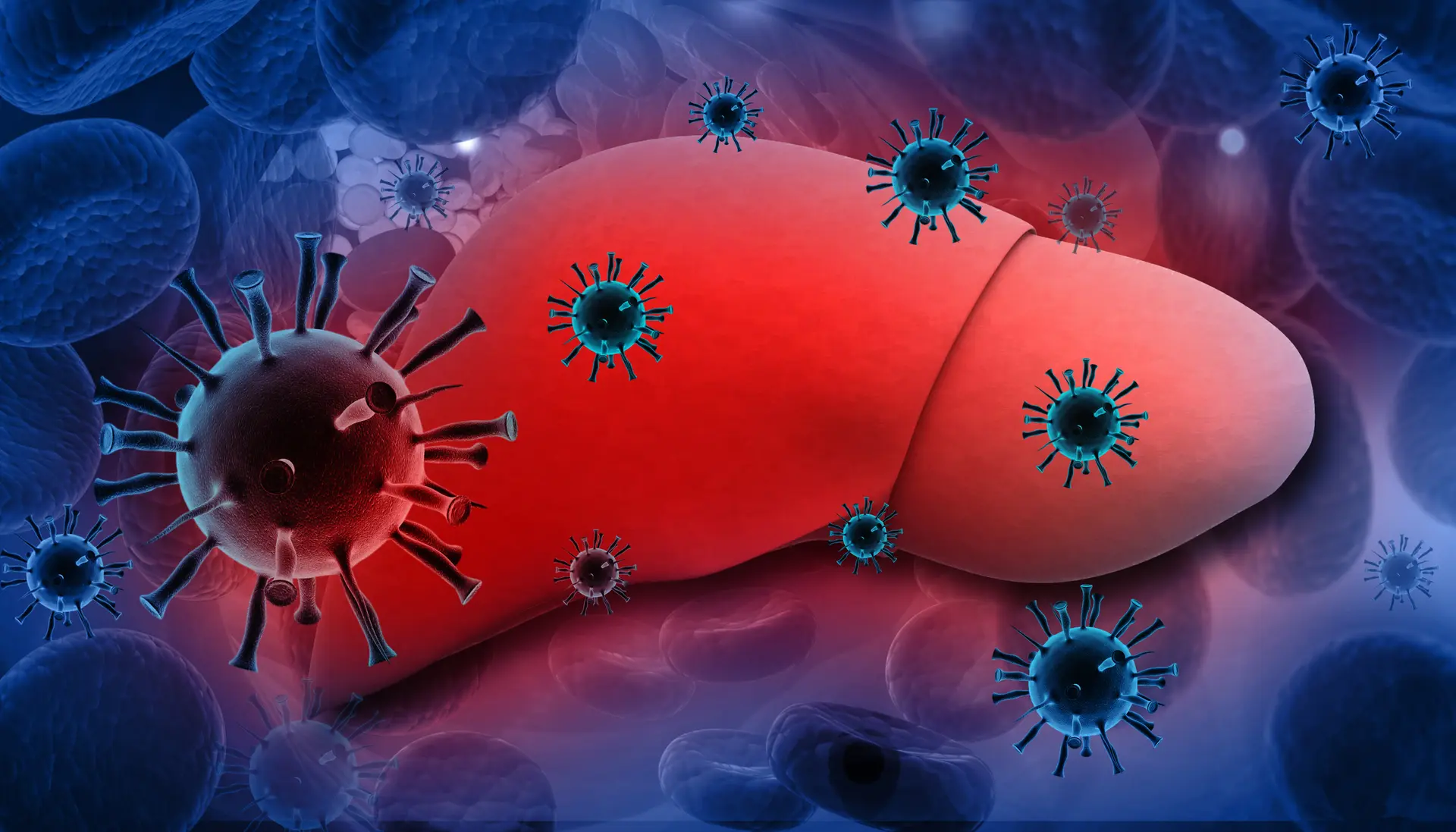
Patient-derived viral contamination has been found in breathing systems and several patients contracted Hepatitis C after using a contaminated breathing circuit.1,2 In 2022 a case was reported, in which an electrostatic, non-hydrophobic breathing filter did not stop the passage of virus-loaded blood and did not prevent the contamination of the breathing circuit and the ventilator with blood-borne Hepatitis C virus.3 Non-hydrophobic electrostatic filters are therefore unable to reliably protect the breathing system against patient contamination. Several laboratory studies confirm this finding4,11,12,13.
Download infographic “Anaesthesia breathing systems”
The Solution
Use of a high efficiency hydrophobic breathing filter has been recommended by professional organizations who suggest only hydrophobic filters can stop the spread of patient derived liquid-borne contamination e.g., blood-borne viruses like Hepatitis C virus and HIV.5-8
Download infographic “Putting a barrier between patient and equipment”
The Proof
The hydrophobic high efficiency Pall Ultipor 25 (BB25) filter has been tested to retain liquid-borne human pathogenic organisms (viral, bacterial, fungal and prion proteins):
- HIV9
- Hepatitis C virus10
- Staphylococcus aureus12
- Infective prion proteins (PrPsc)14
Further laboratory studies have been conducted, which show that the Ultipor 25 also retains Candida albicans11 and Pseudomonas aeruginosa13
Our Products
The safety of patients and healthcare workers is our top priority. To prevent bacterial or viral contamination between patients and breathing systems, we’ve designed a range of high efficiency ventilation and breathing system filters. Get quality filters for anesthesia, intensive care and surgical gas handling.
references
Chant K. et al. (1994). Investigation of possible patient-to-patient transmission of hepatitis C in a hospital. New South Wales Public Health Bulletin 5; 47-51
Heinsen A. et al. (2000). A phylogenetic analysis elucidating a case of patient-to-patient transmission of hepatitis C virus during surgery. J Hosp Inf; 46:309-313
Pel M.E. at al. (2022). Delayed recognition of breathing system contamination with blood containing hepatitis C virus following failure of a heat and moisture exchange filter. Anaesth Rep; 10(1):e12171.
Cann C. et al. (2006). The pressure required to force liquid through breathing system filters. Anaesthesia; 61: 492–497
Kramer A. et al. (2010). Infection prevention during anaesthesia ventilation by the use of breathing system filters (BSF): Joint recommendation by German Society of Hospital Hygiene (DGKH) and German Society for Anaesthesiology and Intensive Care (DGAI). GMS Krankenhhyg Interdiszip; 21:5(2)
Hajjar et al. (2000) Clauses techniques pour l’achat d’un filtre échangeur de chaleur et d’humidité destiné à la ventilation en anesthésie. Ann Fr Anesth Réanim; 19: 556-60
AAGBI Bloodborne virus advisory panel (1996). Possible transmission of Hepatitis C virus (HCV) via the anaesthetic breathing system.
Lloyd G. and Howells J. (1997) Efficacy of a pleated hydrophobic filter as a barrier to human immunodeficiency virus transmission within breathing systems. Centre for Applied Microbiology and Research Report
Lloyd G. et al. (1997). Barriers to hepatitis C transmission within breathing systems: efficacy of a pleated hydrophobic filter. Anaesth Intensive Care; 25(3):235-8
Scott D.H.T. et al. (2010). Passage of pathogenic microorganisms through breathing system filters used in anaesthesia and intensive care. Anaesthesia; 65(7): 670-673
Rosales M. & Dominguez V. (1992) Poster presentation at the 2nd International Conference on Prevention of Infection, Nice, France, 4-5th May 1992
Miorini T. & Wille B. (1990). Hygiene Measures for Anaesthesia and Ventilator Equipment (Correspondence) Krh.-Hyg Inf. Verh. 12: 24
Capewell A. (2004). Prion Retention Properties of PALL Ultipor 25 Breathing System Filters Scientific and Laboratory Services Report Pall Europe

Anaesthesia patient side
Our UltiporTM 25 Breathing Circuit Filter for anesthesia with high efficiency pleated hydrophobic membrane, provides an effective barrier against viruses, bacteria, and liquid-borne contaminants.

Anaesthesia circuits and kits
(Only available with FDA clearance)
Our multi-patient-use breathing circuits can be used between patients for up to 24 hours if every patient is provided with a new Pall UltiporTM 25 breathing circuit filter. This set up is protecting patients, staff, and equipment while increasing efficiency and reducing costs.

Anesthesia and ICU patient side
Our UlitporTM 100 Breathing Circuit Ffilter with high efficiency pleated hydrophobic membrane, provides an effective barrier against viruses, bacteria and liquid-borne contaminants, and ensures physiological humidification of breathing gases. It can also be used for drug nebulization between the filter and the patient.
If no nebulization is used, the service life of UltiporTM 100 can be extended from 24 to 48 hours.

Machine and patient side anesthesia
Our UltiporTM 50 & 55 Breathing Circuit Filter with highly efficient pleated hydrophobic filter medium is designed for ventilator machine side applications and provides an effective barrier for viruses, bacteria, and liquid-borne contaminant. It can also be used as a heat and moisture exchanger filter at patient end in anaesthesia applications.

Highly efficient surgical smoke evacuation
Our LaparoShield® Laparoscopic Smoke Filtration System with ULPA filtration rating and Viral and Bacterial retention, delivers protection for healthcare workers and patients exposed to surgical plume. It is easy to use and works without the need for external pumping equipment.
Insufflation Gas Filtration
Protect your equipment with our IGF1 Insufflator Gas Line Filter (CE Mark) high efficiency hydrophobic filter medium, protecting against microorganism, particles and backflow of bodily fluids and blood.
The products advertised within this website may not have been licensed in accordance with local regulatory laws. Please check with the local Pall office for availability.
Airborne Bacterial and Viral cross-infection
The Problem
Viable Mycobacterium tuberculosis were found in the anesthesia system after exposure to a patient with tuberculosis (TB).1 During the COVID pandemic anesthetists were concerned about anesthesia patients contaminating the anesthesia workstation with the virus.2
Download infographic “Retaining airborne pathogens”
The Solution
Use of a high efficiency hydrophobic breathing filter has been recommended by professional organizations to stop the spread of patient derived contamination and especially human pathogenic organisms.3-6
The Proof
The high efficiency hydrophobic Pall Ultipor 25 filter has been tested to retain airborne human pathogenic organisms:
- SARS-CoV27
- Influenza A8
- Mycobacterium tuberculosis9
Read ourTechnical Report "Filtration Efficiency of the Pall BB50T for SARS-CoV-2"
Our Products
The safety of patients and healthcare workers is our top priority. To prevent bacterial or viral contamination between patients and breathing systems, we’ve designed a range of high efficiency ventilation and breathing system filters. Get quality filters for anesthesia, intensive care and surgical gas handling.

Anaesthesia patient side
Our UltiporTM 25 Breathing Circuit Filter for anesthesia with high efficiency pleated hydrophobic membrane, provides an effective barrier against viruses, bacteria, and liquid-borne contaminants.

Anaesthesia circuits and kits
(Only available with FDA clearance)
Our multi-patient-use breathing circuits can be used between patients for up to 24 hours if every patient is provided with a new Pall UltiporTM 25 breathing circuit filter. This set up is protecting patients, staff, and equipment while increasing efficiency and reducing costs.

Anesthesia and ICU patient side
Our UlitporTM 100 Breathing Circuit Ffilter with high efficiency pleated hydrophobic membrane, provides an effective barrier against viruses, bacteria and liquid-borne contaminants, and ensures physiological humidification of breathing gases. It can also be used for drug nebulization between the filter and the patient.
If no nebulization is used, the service life of UltiporTM 100 can be extended from 24 to 48 hours.

Machine and patient side anesthesia
Our UltiporTM 50 & 55 Breathing Circuit Filter with highly efficient pleated hydrophobic filter medium is designed for ventilator machine side applications and provides an effective barrier for viruses, bacteria, and liquid-borne contaminant. It can also be used as a heat and moisture exchanger filter at patient end in anaesthesia applications.

Highly efficient surgical smoke evacuation
Our LaparoShield® Laparoscopic Smoke Filtration System with ULPA filtration rating and Viral and Bacterial retention, delivers protection for healthcare workers and patients exposed to surgical plume. It is easy to use and works without the need for external pumping equipment.
Insufflation Gas Filtration
Protect your equipment with our IGF1 Insufflator Gas Line Filter (CE Mark) high efficiency hydrophobic filter medium, protecting against microorganism, particles and backflow of bodily fluids and blood.
References
Langevin P.B. et al. (1999). The Potential for Dissemination of Mycobacterium tuberculosis Through the Anesthesia Breathing Circuit. CHEST; 115: 1107-1114
Urdaneta F. & Loeb R.G. (2021). HEPA Filters. Do We Really Know Enough? – Breathing System Filters in the Era of Covid-19APSF Newsletter; 36(1)
Loeb R.G. (2021) Breathing System Filters in the Era of COVID-19 APSF NEWSLETTER February 2021, p. 12-14
Kramer A. et al. (2010). Infection prevention during anaesthesia ventilation by the use of breathing system filters (BSF): Joint recommendation by German Society of Hospital Hygiene (DGKH) and German Society for Anaesthesiology and Intensive Care (DGAI). GMS Krankenhhyg Interdiszip; 21: 5(2)
Hajjar et al. (2000). Clauses techniques pour l’achat d’un filtre échangeur de chaleur et d’humidité destiné à la ventilation en anesthésie. Ann Fr Anesth Réanim ; 19: 556-60
AAGBI Bloodborne virus advisory panel. Possible transmission of Hepatitis C virus (HCV) via the anaesthetic breathing system (1996)
Spiers S. & Quarti C. (2021). Filtration Efficiency of the Pall Ultipor 25 for SARS-CoV-2. Pall SLS Technical Report
Heuer J.F. et al. (2013). Can breathing circuit filters help prevent the spread of influenza A (H1N1) virus from intubated patients? GMS Hyg Infect Control; 29: 8(1)
Speight S. et al. (1995). Efficacy of a pleated hydrophobic filter as a barrier to Mycobacterium tuberculosis transmission within breathing systems. Centre for Applied Microbiology and Research Report.
The products advertised within this website may not have been licensed in accordance with local regulatory laws. Please check with the local Pall office for availability.
Change of the anesthesia breathing circuit is costly, time consuming and creates waste
The Problem

Hospitals are looking to improve efficiency while maintaining or improving cost. The Operating Room (OR) is big area of opportunity, as:
ORs drive up to 60% of a hospital’s revenue1
Are responsible for 40 to 60% of the organization’s total supply costs1
Produce more than 30% of a facility’s waste and two-thirds of its regulated medical waste. 25% of all OR waste has been attributed to anesthesia-related materials1
Read our blog "Greening the operating room"
The Solution
Multi-use anesthesia breathing circuits have been demonstrated to reduce costs by more than $50,000 USD annually for a facility that performs 60 cases a day.2 Overall cost can be reduced to up to 41%.3
Download flyer "Multiple-Patient-use Anesthesia Circuits"
The Proof
A single Pall anesthesia circuit (only available in the US) can be used for all procedures performed within a 24-hour period, if each patient is provided with a fresh Pall patient kit (anesthesia mask, Ultipor 25 heat and moisture exchange filter, elbow adapter).
The key to the ability to reuse circuits is the Pall Ultipor 25 Heat and Moisture Exchange Filter. Rigorous mono-dispersed testing of the hydrophobic Ultipor 25 filter with Brevundimonas diminuta and MS-2 bacteriophage has demonstrated at least 99.999% retention efficiency.4
In addition, Vezina et al. demonstrated superior retention of Mycobacterium chelonae by the Ultipor 25 when compared to other brands of breathing filters.5
Ultipor 25 filtration efficacy is complemented by its patient heat and moisture retention capability. Both Pall dual-limb and coaxial (single-limb) circuit configurations may be reused with Pall patient kits. Based on this validation the Ultipor 25 is registered under CE mark to reduce the risk of cross-contamination and cross infection and to enable the extended use of breathing systems, as per the manufacturers’ instructions.
Read our blog “Multi Use Clinical”
Our Products
The safety of patients and healthcare workers is our top priority. To prevent bacterial or viral contamination between patients and breathing systems, we’ve designed a range of high efficiency ventilation and breathing system filters. Get quality filters for anesthesia, intensive care and surgical gas handling.

Anaesthesia patient side
Our UltiporTM 25 Breathing Circuit Filter for anesthesia with high efficiency pleated hydrophobic membrane, provides an effective barrier against viruses, bacteria, and liquid-borne contaminants.

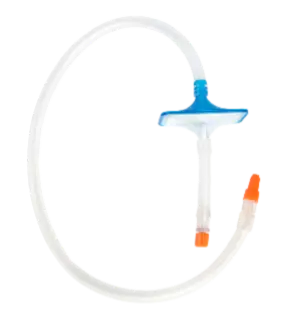
Anaesthesia circuits and kits
(Only available with FDA clearance)
Our multi-patient-use breathing circuits can be used between patients for up to 24 hours if every patient is provided with a new Pall UltiporTM 25 breathing circuit filter. This set up is protecting patients, staff, and equipment while increasing efficiency and reducing costs.

Anesthesia and ICU patient side
Our UlitporTM 100 Breathing Circuit Ffilter with high efficiency pleated hydrophobic membrane, provides an effective barrier against viruses, bacteria and liquid-borne contaminants, and ensures physiological humidification of breathing gases. It can also be used for drug nebulization between the filter and the patient.
If no nebulization is used, the service life of UltiporTM 100 can be extended from 24 to 48 hours.

Machine and patient side anesthesia
Our UltiporTM 50 & 55 Breathing Circuit Filter with highly efficient pleated hydrophobic filter medium is designed for ventilator machine side applications and provides an effective barrier for viruses, bacteria, and liquid-borne contaminant. It can also be used as a heat and moisture exchanger filter at patient end in anaesthesia applications.

Highly efficient surgical smoke evacuation
Our LaparoShield® Laparoscopic Smoke Filtration System with ULPA filtration rating and Viral and Bacterial retention, delivers protection for healthcare workers and patients exposed to surgical plume. It is easy to use and works without the need for external pumping equipment.
Insufflation Gas Filtration
Protect your equipment with our IGF1 Insufflator Gas Line Filter (CE Mark) high efficiency hydrophobic filter medium, protecting against microorganism, particles and backflow of bodily fluids and blood.
References
Greening the OR. Practice Greenhealth. Retrieved March 7, 2023, from https://practicegreenhealth.org/topics/greening-operating-room/greening-or
Daggan R. et al. (1999). High-quality filtration allows reuse of anesthesia breathing circuits resulting in cost savings and reduced medical waste. J Clin Anesth; 11(7):536-539
Hübner N.O. et al. (2011). Microbiological safety and cost-effectiveness of weekly breathing circuit changes in combination with heat moisture exchange filters: a prospective longitudinal clinical survey. GMS Krankenhhyg Interdiszip; 6(1)
Pan L. et al. (1995) Filtration properties of Pall Breathing Circuit Filters (Models BB50T, HME15-22, and BB25A). Pall Technical Report No. BCF2
Vezina D.P. et al. (2004). An in vivo evaluation of the mycobacterial filtration efficiency of three breathing filters used in anesthesia. Anesthesiology; 101(1): 104-109
The products advertised within this website may not have been licensed in accordance with local regulatory laws. Please check with the local Pall office for availability.
Change of anaesthesia circuits generates waste.
The Problem

In healthcare the generation of waste is a known problem. US hospitals produce more than 5.9 million tons of waste each year and 15% of this quantity is considered regulated medical waste.1
Every day, in every OR in the US an average of 4 surgeries are performed, and between 20% and 33% of total hospital waste is attributed to the operating room with 90% of it designated as hazardous material ending up in the red bin.2,3 All the consumables are then either disposed of in a landfill or are incinerated, both of which have environmental impact.
Anesthesia breathing circuits play an important role in this. Many of the components are made of plastic materials (some examples given below) and are considered regulated medical waste:
Circuit
CO2 Gas Sampling Line
Breathing Bag
Mask
Filter
Download infographic “Anesthesia disposables”
The Solution
We have an alternative to using the anesthesia circuits once and then disposing of them. Our Pall Ultipor 25 breathing Circuit Filter and Multiple Patient Use Anesthesia Circuits* allow the circuit to be used repeatedly over a 24-hour period with a new mask and Breathing System Filter used for each patient to prevent cross contamination.
Additionally, these can help to improve efficiency by decreasing turnover times and reduce cost by using fewer circuits per day.
*Available in the USA only
Download infographic “Circuits consumption”
The Proof
A single Pall anesthesia circuit can be used for all procedures performed within a 24-hour period, if each patient is provided with a fresh Pall patient kit (anesthesia mask, Ultipor 25 heat and moisture exchange filter, elbow adapter). The key to the ability to reuse circuits is the Pall Ultipor 25 Heat and Moisture Exchange Filter. Rigorous mono-dispersed testing of the hydrophobic Ultipor 25 filter with Brevundimonas diminuta and MS-2 bacteriophage has demonstrated at least 99.999% retention efficiency.4,5
In addition, Vezina et al. demonstrated superior retention of Mycobacterium chelonae by the Ultipor 25 when compared to other brands of breathing filters.6
The Ultipor 25’s filtration efficacy is complemented by its patient heat and moisture retention capability. Both Pall dual-limb and coaxial (single-limb) circuit configurations may be reused with Pall patient kits.
Read our blog “Reducing Medical Waste”
Our Products
The safety of patients and healthcare workers is our top priority. To prevent bacterial or viral contamination between patients and breathing systems, we’ve designed a range of high efficiency ventilation and breathing system filters. Get quality filters for anesthesia, intensive care and surgical gas handling.

Anaesthesia patient side
Our UltiporTM 25 Breathing Circuit Filter for anesthesia with high efficiency pleated hydrophobic membrane, provides an effective barrier against viruses, bacteria, and liquid-borne contaminants.

Anaesthesia circuits and kits
(Only available with FDA clearance)
Our multi-patient-use breathing circuits can be used between patients for up to 24 hours if every patient is provided with a new Pall UltiporTM 25 breathing circuit filter. This set up is protecting patients, staff, and equipment while increasing efficiency and reducing costs.

Anesthesia and ICU patient side
Our UlitporTM 100 Breathing Circuit Ffilter with high efficiency pleated hydrophobic membrane, provides an effective barrier against viruses, bacteria and liquid-borne contaminants, and ensures physiological humidification of breathing gases. It can also be used for drug nebulization between the filter and the patient.
If no nebulization is used, the service life of UltiporTM 100 can be extended from 24 to 48 hours.

Machine and patient side anesthesia
Our UltiporTM 50 & 55 Breathing Circuit Filter with highly efficient pleated hydrophobic filter medium is designed for ventilator machine side applications and provides an effective barrier for viruses, bacteria, and liquid-borne contaminant. It can also be used as a heat and moisture exchanger filter at patient end in anaesthesia applications.

Highly efficient surgical smoke evacuation
Our LaparoShield® Laparoscopic Smoke Filtration System with ULPA filtration rating and Viral and Bacterial retention, delivers protection for healthcare workers and patients exposed to surgical plume. It is easy to use and works without the need for external pumping equipment.
Insufflation Gas Filtration
Protect your equipment with our IGF1 Insufflator Gas Line Filter (CE Mark) high efficiency hydrophobic filter medium, protecting against microorganism, particles and backflow of bodily fluids and blood.
References
Connelly, D. (2022). How much waste does the healthcare industry produce? All Points Medical Waste. Retrieved March 7, 2023, from https://allpointsmedicalwaste.com/how-much-waste-does-the-healthcare-industry-produce/
Schuster M. et al. (2004). Effect of Different Cost Drivers on Cost per Anesthesia Minute in Different Anesthesia Subspecialties. Anesthesiology; 101: 1435-43
Blough C.L. & Karsh K.J. (2021). What’s Important: Operating Room Waste - Why We Should Care. The Journal of Bone and Joint Surgery; 103(9): 837-839
Pan L. et al. (1995). Filtration Properties of Pall Breathing Circuit Filters (Models BB50T, HME15-22, and BB25A). Pall Technical Report No. BCF2
Vezina D.P. et al. (2004). An in vivo evaluation of the mycobacterial filtration efficacy of three breathing filters used in anesthesia. Anesthesiology; 101(1):104-9
The products advertised within this website may not have been licensed in accordance with local regulatory laws. Please check with the local Pall office for availability.
Anaesthesia consumables are costly and disposable
The Problem

Hospitals and Health Systems have experienced an increase in expense per patient of around 20.1% over the last few years. Hospital departments most directly involved in COVID-19 patients care such as ICUs and respiratory care departments have seen medical supply expenses increase by 31.5% and 22.3%, respectively, from pre-pandemic levels.1 Institutions are therefore looking to improve efficiency while maintaining or even improving cost without impacting clinical outcomes.
One key area of concern is the operating room (OR)2:
ORs drive up to 60% of a hospital’s revenue
Are responsible for 40 to 60% of the organization’s total supply costs
Produce more than 30% of a facility’s waste and two-thirds of its regulated medical waste
25% of all OR waste has been attributed to anesthesia-related materials
Read our Blog "Multi - use - Economics"
The Solution
We have an alternative to using the anesthesia circuits once and then disposing of them. Our Pall Ultipor 25 breathing System Filter and Multiple Patient Use Anesthesia Circuits* allow the circuit to be used repeatedly over a 24-hour period with a new mask and Breathing System Filter used for each patient to prevent cross contamination.
Additionally, these can help to improve efficiency by decreasing turnover times and reduce cost by using fewer circuits per day.
Download flyer "Multiple-Patient-use Anesthesia Circuits"
The Proof
Studies have shown savings of up to $50,000 per year by extending the use of the anesthesia circuits from single patient use to 24 h where possible and under certain conditions in a facility with about 60 cases performed under general anesthesia per day.3,4
Extending the use of the anesthesia circuits can be achieved with the High Efficiency Heat Moisture Exchange Filter Pall Ultipor 25 Breathing Circuit Filter used in conjunction with the Pall Multiuse anesthesia circuits*. The hydrophobic Pall Ultipor 25 Breathing Circuit Filter is a safe and effective barrier against both liquid-borne and airborne patient-derived contamination and protects the interior of the breathing circuit. The Pall Ultipor Anesthesia Breathing Circuit System* has been cleared by the FDA under 510k registration, supporting the ability of the circuit to be used across multiple patients for up to 24 h if a new Ultipor 25 Breathing Circuit Filter is used and changed after each patient.
*Available in the USA only
Read our Blog "Multi - use - Economics"
Our Products
The safety of patients and healthcare workers is our top priority. To prevent bacterial or viral contamination between patients and breathing systems, we’ve designed a range of high efficiency ventilation and breathing system filters. Get quality filters for anesthesia, intensive care and surgical gas handling.

Anaesthesia patient side
Our UltiporTM 25 Breathing Circuit Filter for anesthesia with high efficiency pleated hydrophobic membrane, provides an effective barrier against viruses, bacteria, and liquid-borne contaminants.

Anaesthesia circuits and kits
(Only available with FDA clearance)
Our multi-patient-use breathing circuits can be used between patients for up to 24 hours if every patient is provided with a new Pall UltiporTM 25 breathing circuit filter. This set up is protecting patients, staff, and equipment while increasing efficiency and reducing costs.

Anesthesia and ICU patient side
Our UlitporTM 100 Breathing Circuit Ffilter with high efficiency pleated hydrophobic membrane, provides an effective barrier against viruses, bacteria and liquid-borne contaminants, and ensures physiological humidification of breathing gases. It can also be used for drug nebulization between the filter and the patient.
If no nebulization is used, the service life of UltiporTM 100 can be extended from 24 to 48 hours.

Machine and patient side anesthesia
Our UltiporTM 50 & 55 Breathing Circuit Filter with highly efficient pleated hydrophobic filter medium is designed for ventilator machine side applications and provides an effective barrier for viruses, bacteria, and liquid-borne contaminant. It can also be used as a heat and moisture exchanger filter at patient end in anaesthesia applications.

Highly efficient surgical smoke evacuation
Our LaparoShield® Laparoscopic Smoke Filtration System with ULPA filtration rating and Viral and Bacterial retention, delivers protection for healthcare workers and patients exposed to surgical plume. It is easy to use and works without the need for external pumping equipment.
Insufflation Gas Filtration
Protect your equipment with our IGF1 Insufflator Gas Line Filter (CE Mark) high efficiency hydrophobic filter medium, protecting against microorganism, particles and backflow of bodily fluids and blood.
References
American Hospital Association. (2022). Massive Growth in Expenses and Rising Inflation Fuel Continued Financial Challenges for America’s Hospitals and Health Systems. Retrieved March 7, 2023, from https://www.aha.org/system/files/media/file/2022/04/2022-Hospital-Expenses-Increase-Report-Final-Final.pdf
Connelly, D. (2022). How much waste does the healthcare industry produce? All points. All Points Medical Waste. Retrieved March 7, 2023, from https://allpointsmedicalwaste.com/how-much-waste-does-the-healthcare-industry-produce/
Egger Halbeis C.B. et al. (2008). The reuse of anesthesia breathing systems: another difference of opinion and practice between the United States and Europe. J Clin Anesth; 20(2):81-3
Daggan R. et al. (1999). High-quality filtration allows reuse of anesthesia breathing circuits resulting in cost savings and reduced medical waste. J Clin Anesth; 11(7):536-9
The products advertised within this website may not have been licensed in accordance with local regulatory laws. Please check with the local Pall office for availability.
More than half a million health care workers exposed to surgical smoke every year
The Problem

Surgical smoke is not only a nuisance because of the vision obstruction to surgeons and its noxious odor, it also puts the entire surgical staff’s health at risk. Surgical smoke is a mix of water vapor, volatile gaseous compounds, and particles derived from the degradation of tissue during laser and electrocautery surgeries. Among the substances found in surgical smoke are toxic, teratogenic, and carcinogenic chemicals. It may also contain viable viruses and cellular material. Chronic exposure to surgical smoke is a concern for healthcare professionals working in a confined space of the Operating Room (OR) where the constituents of the smoke can be inhaled and absorbed through the lungs. Surgical smoke is also harmful to the patient, as it can be absorbed via the peritoneum and cause nausea or a longer recovery time.1
Download infographic "Smoke Production in Laparoscopic Surgery
The Solution
The Pall LaparoShield® Laparoscopic Smoke Filtration System is an easy-to-use passive smoke evacuation system which removes, bacteria, viruses and odor causing noxious chemicals from surgical smoke generated in laparoscopic procedures while maintaining a clear field of vision. It has also been validated to retain particles at ULPA-rated efficienciency.3 The universal luer connector meets ISO standards for leak free connection to the trocar. The LaparoShield is indicated for use during any minimally invasive surgery involving insufflation, electrocautery, laser, or ultrasonic scalpel use. The lightweight, low-profile construction makes efficient use of materials providing a non-obtrusive, cost-effective solution to laparoscopic smoke removal. It is also packaged in a sterile double peel-pouch allowing easy presentation into the sterile field.
Download flyer “Laparoshield® Laparoscopic Smoke Filters”
Download infographic “Surgical smoke should be filtered”
The Proof
Clinical as well as laboratory studies have shown that the LaparoShield filter retains harmful volatile chemicals, viruses, bacteria, and particles (ULPA filtration rating).2,3
“Smoke-free”-policies are promoted by professional organizations and adopted by more and more lawmakers across the USA.4,5
Our Products
The safety of patients and healthcare workers is our top priority. To prevent bacterial or viral contamination between patients and breathing systems, we’ve designed a range of high efficiency ventilation and breathing system filters. Get quality filters for anesthesia, intensive care and surgical gas handling.

Anaesthesia patient side
Our UltiporTM 25 Breathing Circuit Filter for anesthesia with high efficiency pleated hydrophobic membrane, provides an effective barrier against viruses, bacteria, and liquid-borne contaminants.

Anaesthesia circuits and kits
(Only available with FDA clearance)
Our multi-patient-use breathing circuits can be used between patients for up to 24 hours if every patient is provided with a new Pall UltiporTM 25 breathing circuit filter. This set up is protecting patients, staff, and equipment while increasing efficiency and reducing costs.

Anesthesia and ICU patient side
Our UlitporTM 100 Breathing Circuit Ffilter with high efficiency pleated hydrophobic membrane, provides an effective barrier against viruses, bacteria and liquid-borne contaminants, and ensures physiological humidification of breathing gases. It can also be used for drug nebulization between the filter and the patient.
If no nebulization is used, the service life of UltiporTM 100 can be extended from 24 to 48 hours.

Machine and patient side anesthesia
Our UltiporTM 50 & 55 Breathing Circuit Filter with highly efficient pleated hydrophobic filter medium is designed for ventilator machine side applications and provides an effective barrier for viruses, bacteria, and liquid-borne contaminant. It can also be used as a heat and moisture exchanger filter at patient end in anaesthesia applications.

Highly efficient surgical smoke evacuation
Our LaparoShield® Laparoscopic Smoke Filtration System with ULPA filtration rating and Viral and Bacterial retention, delivers protection for healthcare workers and patients exposed to surgical plume. It is easy to use and works without the need for external pumping equipment.
Insufflation Gas Filtration
Protect your equipment with our IGF1 Insufflator Gas Line Filter (CE Mark) high efficiency hydrophobic filter medium, protecting against microorganism, particles and backflow of bodily fluids and blood.
References
Alp E. et al. (2006). Surgical smoke and infection control. Journal of Hospital Infection; 62: 1-5
Nolde J. et al. (2002). On the necessity of using desufflation gas filters during laparoscopic surgery: Quantitative analysis of coagulation gas metabolites. Poster presentation at the 4th Annual Congress of the CAMIC, Heidelberg, Germany
Stephens A. et al. (2001). Bacterial and Viral Retention of the Pall LaparoShield Laparoscopic Smoke Filtration System. Pall SLS Technical Report CC78
Healthcare Purchasing News. (2021). Oregon state to ensure smoke-free operating rooms. Retrieved March 7, 2023, from https://www.hpnonline.com/surgical-critical-care/article/21229521/oregon-state-to-ensure-smokefree-operating-rooms
AORN (2021) Smoke Evacuation News. Published: 1/25/2021 https://www.aorn.org/article/2021-01-25-Smoke-Evacuation-News
The products advertised within this website may not have been licensed in accordance with local regulatory laws. Please check with the local Pall office for availability.
Surgical smoke may contain viruses
The Problem

Surgical Smoke produced by the thermal destruction of the tissue using lasers or electrosurgical devices, has revealed the presence of large particles and viable viruses, like, Human Immunodeficiency virus (HIV) and Human Papillomavirus (HPV) with reports of Operating Room staff turning positive for such virus.1-3
The Solution
The Pall LaparoShield® Laparoscopic Smoke Filtration system protects staff and patients from chemical, particulate and biological contamination with a virus, cellular and bacterial efficiency > 99.999% using Brevundimonas diminuta and MS2 bacteriophage as the test organisms. It is easy to use and does not require an additional pump.
Download flyer “Laparoshield® Laparoscopic Smoke Filters”
The Proof
Society of American Gastrointestinal Endoscopic Surgeons (SAGES), latest guidelines for laparoscopic procedures during covid-19 era recommends that measures, such as viral filters, should be employed for all minimally invasive cases to prevent exposure of operating room staff to the surgical plume.
Our Products
The safety of patients and healthcare workers is our top priority. To prevent bacterial or viral contamination between patients and breathing systems, we’ve designed a range of high efficiency ventilation and breathing system filters. Get quality filters for anesthesia, intensive care and surgical gas handling.

Anaesthesia patient side
Our UltiporTM 25 Breathing Circuit Filter for anesthesia with high efficiency pleated hydrophobic membrane, provides an effective barrier against viruses, bacteria, and liquid-borne contaminants.

Anaesthesia circuits and kits
(Only available with FDA clearance)
Our multi-patient-use breathing circuits can be used between patients for up to 24 hours if every patient is provided with a new Pall UltiporTM 25 breathing circuit filter. This set up is protecting patients, staff, and equipment while increasing efficiency and reducing costs.

Anesthesia and ICU patient side
Our UlitporTM 100 Breathing Circuit Ffilter with high efficiency pleated hydrophobic membrane, provides an effective barrier against viruses, bacteria and liquid-borne contaminants, and ensures physiological humidification of breathing gases. It can also be used for drug nebulization between the filter and the patient.
If no nebulization is used, the service life of UltiporTM 100 can be extended from 24 to 48 hours.

Machine and patient side anesthesia
Our UltiporTM 50 & 55 Breathing Circuit Filter with highly efficient pleated hydrophobic filter medium is designed for ventilator machine side applications and provides an effective barrier for viruses, bacteria, and liquid-borne contaminant. It can also be used as a heat and moisture exchanger filter at patient end in anaesthesia applications.

Highly efficient surgical smoke evacuation
Our LaparoShield® Laparoscopic Smoke Filtration System with ULPA filtration rating and Viral and Bacterial retention, delivers protection for healthcare workers and patients exposed to surgical plume. It is easy to use and works without the need for external pumping equipment.
Insufflation Gas Filtration
Protect your equipment with our IGF1 Insufflator Gas Line Filter (CE Mark) high efficiency hydrophobic filter medium, protecting against microorganism, particles and backflow of bodily fluids and blood.
References
Baggish M.S. et al. (1991). Presence of human immunodeficiency virus DNA in laser smoke. Lasers Surg Med; 11(3): 197-203
Rioux M. et al. (2013). HPV positive tonsillar cancer in two laser surgeons: case reports. J Otolaryngol Head Neck Surg; 42(1): 54
Collings A. T. et al. (2022). 2022 guidance statement regarding the use of laparoscopy in the era of COVID-19 - a sages publication. SAGES. Retrieved March 7, 2023, from https://www.sages.org/publications/guidelines/guidance-statement-regarding-the-use-of-laparoscopy-in-the-era-of-covid-19/
The products advertised within this website may not have been licensed in accordance with local regulatory laws. Please check with the local Pall office for availability.
Smoke obscures the vision on the surgical field
The Problem

A continually clear surgical field of view is critical to efficient surgical procedure turnover.1,2 Waiting for surgical smoke to spontaneously dissipate or having to resort to desufflating the pneumoperitoneum to clear the field of view unnecessarily lengthens procedures and exposes the patient and healthcare personnel to health risks. In addition, poor visibility can lead to surgical team distraction, frustration, and procedural errors.
The Solution
The Pall LaparoShield® Laparoscopic Smoke Filtration System enables continual gas flow to purge surgical smoke during procedures that require extensive use of electrocautery or lasers. Interruption of surgical procedures due to vision impairment is avoided, and overall procedure time is decreased.
Download flyer “Laparoshield® Laparoscopic Smoke Filters”
The Proof
Maintain a constant desufflation to enable continuers gas flow and prevent the reduction of visibility in the surgical field.
Our Products
The safety of patients and healthcare workers is our top priority. To prevent bacterial or viral contamination between patients and breathing systems, we’ve designed a range of high efficiency ventilation and breathing system filters. Get quality filters for anesthesia, intensive care and surgical gas handling.

Anaesthesia patient side
Our UltiporTM 25 Breathing Circuit Filter for anesthesia with high efficiency pleated hydrophobic membrane, provides an effective barrier against viruses, bacteria, and liquid-borne contaminants.

Anaesthesia circuits and kits
(Only available with FDA clearance)
Our multi-patient-use breathing circuits can be used between patients for up to 24 hours if every patient is provided with a new Pall UltiporTM 25 breathing circuit filter. This set up is protecting patients, staff, and equipment while increasing efficiency and reducing costs.

Anesthesia and ICU patient side
Our UlitporTM 100 Breathing Circuit Ffilter with high efficiency pleated hydrophobic membrane, provides an effective barrier against viruses, bacteria and liquid-borne contaminants, and ensures physiological humidification of breathing gases. It can also be used for drug nebulization between the filter and the patient.
If no nebulization is used, the service life of UltiporTM 100 can be extended from 24 to 48 hours.

Machine and patient side anesthesia
Our UltiporTM 50 & 55 Breathing Circuit Filter with highly efficient pleated hydrophobic filter medium is designed for ventilator machine side applications and provides an effective barrier for viruses, bacteria, and liquid-borne contaminant. It can also be used as a heat and moisture exchanger filter at patient end in anaesthesia applications.

Highly efficient surgical smoke evacuation
Our LaparoShield® Laparoscopic Smoke Filtration System with ULPA filtration rating and Viral and Bacterial retention, delivers protection for healthcare workers and patients exposed to surgical plume. It is easy to use and works without the need for external pumping equipment.
Insufflation Gas Filtration
Protect your equipment with our IGF1 Insufflator Gas Line Filter (CE Mark) high efficiency hydrophobic filter medium, protecting against microorganism, particles and backflow of bodily fluids and blood.
References
Weld K.J. et al. (2007). Analysis of surgical smoke produced by various energy-based instruments and effect on laparoscopic visibility. J Endourol; 21(3):347-51
Barrett W.L. & Garber S.M. (2003). Surgical smoke: a review of the literature. Is this just a lot of hot air? Surg Endosc; 17(6):979-87
The products advertised within this website may not have been licensed in accordance with local regulatory laws. Please check with the local Pall office for availability.
Surgical smoke contains respirable dust (small particles <2.5µm)
The Problem

During endosurgical procedures electro-surgical scalpels and laser-instruments create high amounts of respirable particles which can get inhaled by surgical staff. Solid fine particulate matter with a diameter smaller than 2.5 μm (PM2.5) gets deposited in the alveolar region of the lung, where the only clearance mechanism consists of phagocytosis by alveolar macrophages and transfer into the circulatory system.1 Long term exposure to PM2.5 has been associated with an increased risk of dying from myocardial infarction, ischemic heart disease, stroke, and are also tied to a series of cognitive and mental outcomes, including depression2,3,4.
The Solution
The use of the high efficiency filter Pall LaparoShield Smoke Filtration System® on a desufflation trocar will retain particles in the PM2.5 size range and protect surgical staff against the inhalation of PM 2.5
The Proof
“During endoscopic surgery smoke is accumulated and released at once in a relatively high velocity air flow. Surgeons should pay attention that the jet is not pointed at persons standing close. The preferred preventive measure would be to use a commercially available filter that can be attached to the Luer lock valve on the cannula and that removes cells, particulates, and chemical gases when desufflating.”1
The Pall LaparoShield Smoke Filtration System has been validated as an Ultra Low Penetration Air Filter (ULPA-rating)5
Our Products
The safety of patients and healthcare workers is our top priority. To prevent bacterial or viral contamination between patients and breathing systems, we’ve designed a range of high efficiency ventilation and breathing system filters. Get quality filters for anesthesia, intensive care and surgical gas handling.

Anaesthesia patient side
Our UltiporTM 25 Breathing Circuit Filter for anesthesia with high efficiency pleated hydrophobic membrane, provides an effective barrier against viruses, bacteria, and liquid-borne contaminants.

Anaesthesia circuits and kits
(Only available with FDA clearance)
Our multi-patient-use breathing circuits can be used between patients for up to 24 hours if every patient is provided with a new Pall UltiporTM 25 breathing circuit filter. This set up is protecting patients, staff, and equipment while increasing efficiency and reducing costs.

Anesthesia and ICU patient side
Our UlitporTM 100 Breathing Circuit Ffilter with high efficiency pleated hydrophobic membrane, provides an effective barrier against viruses, bacteria and liquid-borne contaminants, and ensures physiological humidification of breathing gases. It can also be used for drug nebulization between the filter and the patient.
If no nebulization is used, the service life of UltiporTM 100 can be extended from 24 to 48 hours.

Machine and patient side anesthesia
Our UltiporTM 50 & 55 Breathing Circuit Filter with highly efficient pleated hydrophobic filter medium is designed for ventilator machine side applications and provides an effective barrier for viruses, bacteria, and liquid-borne contaminant. It can also be used as a heat and moisture exchanger filter at patient end in anaesthesia applications.

Highly efficient surgical smoke evacuation
Our LaparoShield® Laparoscopic Smoke Filtration System with ULPA filtration rating and Viral and Bacterial retention, delivers protection for healthcare workers and patients exposed to surgical plume. It is easy to use and works without the need for external pumping equipment.
Insufflation Gas Filtration
Protect your equipment with our IGF1 Insufflator Gas Line Filter (CE Mark) high efficiency hydrophobic filter medium, protecting against microorganism, particles and backflow of bodily fluids and blood.
References
Brüske-Hohlfeld I. et al. (2008). Surgical smoke and ultrafine particles. Journal of Occupational Medicine and Toxicology; 3:31
Alexeeff S.E. et al. Long-term PM2.5 exposure and risks of ischemic heart disease and stroke events: review and meta-analysis. J Am Heart Assoc. 2021;10(1):e016890
Alexeeff S.E. et al. (2023) Association of Long-term Exposure to Particulate Air Pollution With Cardiovascular Events in California. JAMA Network Open. 2023;6(2):e230561
Qiu X. et al. (2023) Association of Long-term Exposure to Air Pollution With Late-Life Depression in Older Adults in the US. JAMA Network Open. 2023;6(2):e2253668.
The products advertised within this website may not have been licensed in accordance with local regulatory laws. Please check with the local Pall office for availability.
10% - 20% of patients suffer from VAP¹
The Problem

Mechanical ventilation in ICU is associated with a high risk of acquiring VAP. Mortality depends on many factors and a fast and specific antibiotic treatment is crucial once the infection has been diagnosed. If treatment is delayed and not adequate, mortality may be as high as 90%.2 VAP originates mainly from endogenous sources.
The Solution
Among many other measures, preventative strategies must keep the lung in a healthy state, e.g., by protecting the mucociliary clearance in conjunction with good tracheal care. Exogenous contamination (e.g. bacterial or viral contamination of water condensate) must be avoided.
The Proof
In a meta-analysis passive humidification has been shown to give better outcomes on VAP as compared to active humidification.3
A randomized clinical study showed that the study group provided with a Pall BB100 (a first-generation housing variant of the Ultipor 100) had a 9% lower incidence of VAP than patients treated with active humidification.4
Our Products
The safety of patients and healthcare workers is our top priority. To prevent bacterial or viral contamination between patients and breathing systems, we’ve designed a range of high efficiency ventilation and breathing system filters. Get quality filters for anesthesia, intensive care and surgical gas handling.

Anaesthesia patient side
Our UltiporTM 25 Breathing Circuit Filter for anesthesia with high efficiency pleated hydrophobic membrane, provides an effective barrier against viruses, bacteria, and liquid-borne contaminants.

Anaesthesia circuits and kits
(Only available with FDA clearance)
Our multi-patient-use breathing circuits can be used between patients for up to 24 hours if every patient is provided with a new Pall UltiporTM 25 breathing circuit filter. This set up is protecting patients, staff, and equipment while increasing efficiency and reducing costs.

Anesthesia and ICU patient side
Our UlitporTM 100 Breathing Circuit Ffilter with high efficiency pleated hydrophobic membrane, provides an effective barrier against viruses, bacteria and liquid-borne contaminants, and ensures physiological humidification of breathing gases. It can also be used for drug nebulization between the filter and the patient.
If no nebulization is used, the service life of UltiporTM 100 can be extended from 24 to 48 hours.

Machine and patient side anesthesia
Our UltiporTM 50 & 55 Breathing Circuit Filter with highly efficient pleated hydrophobic filter medium is designed for ventilator machine side applications and provides an effective barrier for viruses, bacteria, and liquid-borne contaminant. It can also be used as a heat and moisture exchanger filter at patient end in anaesthesia applications.

Highly efficient surgical smoke evacuation
Our LaparoShield® Laparoscopic Smoke Filtration System with ULPA filtration rating and Viral and Bacterial retention, delivers protection for healthcare workers and patients exposed to surgical plume. It is easy to use and works without the need for external pumping equipment.
Insufflation Gas Filtration
Protect your equipment with our IGF1 Insufflator Gas Line Filter (CE Mark) high efficiency hydrophobic filter medium, protecting against microorganism, particles and backflow of bodily fluids and blood.
References
Hellyer T.P. et al. (2016). The Intensive Care Society recommended bundle of interventions for the prevention of ventilator-associated pneumonia. J Intensive Care Soc; 17(3):238-243
Torres A. et al. (2017). ERS/ESICM/ESCMID/ALAT guidelines for the management of hospital-acquired pneumonia and ventilator-associated pneumonia. Eur Respir J; 50:1700582
Kola A. et al. (2005). Efficacy of heat and moisture exchangers in preventing ventilator-associated pneumonia: meta-analysis of randomized controlled trials. Intensive Care Med; 31:5-11
Kirton O et al. (1997). A Prospective, Randomized Comparison of an In-Line Heat Moisture Exchange Filter and Heated Wire Humidifiers* Rates of Ventilator-Associated Early-Onset (Community-Acquired) or Late-Onset (Hospital-Acquired) Pneumonia and Incidence of Endotracheal Tube Occlusion. Chest; 112:1055-1059
The products advertised within this website may not have been licensed in accordance with local regulatory laws. Please check with the local Pall office for availability.
Intubation bypasses upper airways and can lead to lung damage and pneumonia
The Problem
Healthy individuals lose approximately 7 – 12 mg of water from their lungs per liter of gas they exhale. Our nose and upper respiratory tract will provide the heat and humidity to keep this heat and humidity loss within the physiological range. Most ventilated ICU patients will need to get intubated, and their endotracheal tube bypasses the upper airways, depriving them of their humidification function for the cold and dry inspiration gases. If no countermeasures are taken the mucus membranes of the lower respiratory tract will lose its capability to cleanse the lung of contamination via the mucociliary clearance mechanism as they dry out gradually. Lung secreta and microbiological contamination will then be retained within the lungs, increasing the risk for pneumonia.
Over-humidifying by adding too much water to the inspiration gases may have the same effect and can impair the mucociliary clearance function of the lung.
The Solution
Intubated patients in ICU need external artificial humidification of the ventilation gases to keep their lungs in a healthy, physiological state. Either an active humidifier system or a (passive) heat and moisture exchanger (HME) can be used for this purpose. In addition to their HME-function devices may also have a filtering function (HME-filter). HME(Filters) will retain most of the humidity and heat from the patient’s exhaled gases and ad it back to the ventilation gases of the next inspiration.
The goal of artificial airway humidification is to restore the physiological water loss of the patient to 7 – 12 mg/L. Depending on the humidity in the ventilation gases this will require that the artificial humidifier – passive or active – will supply up to 37 mg of water per liter to the inspiration gases.
The Proof
As opposed to active humidifiers, HMEs and HME-Filters are unlikely to over-humidify breathing gases. They have been shown to preserve the physiological and rheological properties of the respiratory mucus and have also been associated with better patient outcomes in clinical studies on ventilator associated pneumonia (VAP).1-3 This is also supported by a Cochrane analysis.4 HMEFs are easy to install, and a clinical study with the Pall BB100 lead to a cost-reduction in consumable products of > 54 % and ventilator days on patients with VAP by >37 %.3
Our Products
The safety of patients and healthcare workers is our top priority. To prevent bacterial or viral contamination between patients and breathing systems, we’ve designed a range of high efficiency ventilation and breathing system filters. Get quality filters for anesthesia, intensive care and surgical gas handling.

Anaesthesia patient side
Our UltiporTM 25 Breathing Circuit Filter for anesthesia with high efficiency pleated hydrophobic membrane, provides an effective barrier against viruses, bacteria, and liquid-borne contaminants.

Anaesthesia circuits and kits
(Only available with FDA clearance)
Our multi-patient-use breathing circuits can be used between patients for up to 24 hours if every patient is provided with a new Pall UltiporTM 25 breathing circuit filter. This set up is protecting patients, staff, and equipment while increasing efficiency and reducing costs.

Anesthesia and ICU patient side
Our UlitporTM 100 Breathing Circuit Ffilter with high efficiency pleated hydrophobic membrane, provides an effective barrier against viruses, bacteria and liquid-borne contaminants, and ensures physiological humidification of breathing gases. It can also be used for drug nebulization between the filter and the patient.
If no nebulization is used, the service life of UltiporTM 100 can be extended from 24 to 48 hours.

Machine and patient side anesthesia
Our UltiporTM 50 & 55 Breathing Circuit Filter with highly efficient pleated hydrophobic filter medium is designed for ventilator machine side applications and provides an effective barrier for viruses, bacteria, and liquid-borne contaminant. It can also be used as a heat and moisture exchanger filter at patient end in anaesthesia applications.

Highly efficient surgical smoke evacuation
Our LaparoShield® Laparoscopic Smoke Filtration System with ULPA filtration rating and Viral and Bacterial retention, delivers protection for healthcare workers and patients exposed to surgical plume. It is easy to use and works without the need for external pumping equipment.
Insufflation Gas Filtration
Protect your equipment with our IGF1 Insufflator Gas Line Filter (CE Mark) high efficiency hydrophobic filter medium, protecting against microorganism, particles and backflow of bodily fluids and blood.
References
Nakagawa N.K. et al. (2000). Effects of a heat and moisture exchanger and a heated humidifier on respiratory mucus in patients undergoing mechanical ventilation. Critical Care Medicine; 28(2):312-317
Kola A. et al. (2005). Efficacy of heat and moisture exchangers in preventing ventilator-associated pneumonia: meta-analysis of randomized controlled trials. Intensive Care Med; 31:5-11
Kirton O. et al. (1997). A Prospective, Randomized Comparison of an In-Line Heat Moisture Exchange Filter and Heated Wire Humidifiers* Rates of Ventilator-Associated Early-Onset (Community-Acquired) or Late-Onset (Hospital-Acquired) Pneumonia and Incidence of Endotracheal Tube Occlusion. Chest; 112:1055-1059
Kelly M. et al. (2012). Heated humidification versus heat and moisture exchangers for ventilated adults and children. The Cochrane Library; 8
The products advertised within this website may not have been licensed in accordance with local regulatory laws. Please check with the local Pall office for availability.
Nebulized drugs can damage ventilators and contaminate the ICU environment
The Problem

Nebulization of drugs is an accepted practice to provide targeted treatment to ventilated patients’ lungs.¹ Unfortunately, this can lead to health care professionals being exposed to the very drugs they are using to treat patients. This unwanted exposure can lead to health care professionals (particularly respiratory therapists) developing occupational asthma after entering the profession², and damage to the ventilator itself.
The Solution
The Pall Ultipor 100 filter (position A in picture below) is compatible with the use of a drug nebulizer (2) between the patient side filter and the patient’s endotracheal tube. It ensures that the ventilator is not damaged and that health care professionals are not exposed to the nebulized drug products.
The Proof
During a study that compared the levels of secondhand aerosol exposure between systems with and without and expiratory filter it was concluded that without a filter exposure was between 40% and 45% of the drug load. Utilizing a pleated hydrophobic mechanical filter reduced this to 0.25%, whereas other types of filters were between 9 and 24 times less efficient (2.2 – 6.1% of drug aerosol passing to ambient.2 The Pall Ultipor 100 Filter has been validated as HEPA-grade filter3 and was tested as per ISO 23328 with 0.3µm NaCl particles. It came out as the best filter among 104 products available in the market.4
Our Products
The safety of patients and healthcare workers is our top priority. To prevent bacterial or viral contamination between patients and breathing systems, we’ve designed a range of high efficiency ventilation and breathing system filters. Get quality filters for anesthesia, intensive care and surgical gas handling.

Anaesthesia patient side
Our UltiporTM 25 Breathing Circuit Filter for anesthesia with high efficiency pleated hydrophobic membrane, provides an effective barrier against viruses, bacteria, and liquid-borne contaminants.

Anaesthesia circuits and kits
(Only available with FDA clearance)
Our multi-patient-use breathing circuits can be used between patients for up to 24 hours if every patient is provided with a new Pall UltiporTM 25 breathing circuit filter. This set up is protecting patients, staff, and equipment while increasing efficiency and reducing costs.

Anesthesia and ICU patient side
Our UlitporTM 100 Breathing Circuit Ffilter with high efficiency pleated hydrophobic membrane, provides an effective barrier against viruses, bacteria and liquid-borne contaminants, and ensures physiological humidification of breathing gases. It can also be used for drug nebulization between the filter and the patient.
If no nebulization is used, the service life of UltiporTM 100 can be extended from 24 to 48 hours.

Machine and patient side anesthesia
Our UltiporTM 50 & 55 Breathing Circuit Filter with highly efficient pleated hydrophobic filter medium is designed for ventilator machine side applications and provides an effective barrier for viruses, bacteria, and liquid-borne contaminant. It can also be used as a heat and moisture exchanger filter at patient end in anaesthesia applications.

Highly efficient surgical smoke evacuation
Our LaparoShield® Laparoscopic Smoke Filtration System with ULPA filtration rating and Viral and Bacterial retention, delivers protection for healthcare workers and patients exposed to surgical plume. It is easy to use and works without the need for external pumping equipment.
Insufflation Gas Filtration
Protect your equipment with our IGF1 Insufflator Gas Line Filter (CE Mark) high efficiency hydrophobic filter medium, protecting against microorganism, particles and backflow of bodily fluids and blood.
References
Dhanani J. et al. (2016). Fundamentals of aerosol therapy in critical care. Crit Care 20, 269 (2016). Fugitive aerosols in the intensive care unit: a narrative review. Ann Transl Med; 9(7): 592
Ari A. et al. (2016). Secondhand aerosol exposure during mechanical ventilation with and without expiratory filters: An in-vitro study. Ind J Resp Care; 5(1): 677-82
Wilkes A.R. (2004). Breathing System Filters. MHRA Evaluation Report 04005
The products advertised within this website may not have been licensed in accordance with local regulatory laws. Please check with the local Pall office for availability.
Patients release aerosols loaded with viruses and bacteria, which can contaminate the ambient air and cause infection1
The Problem
Respiratory therapists, nurses, health care workers, patients and families are exposed to a variety of infectious agents and aerosolized medications in the health care environment.1,2
The Solution
The use of a high efficiency bacterial and viral filter will stop respiratory aerosols either at the patient’s endotracheal tube or at the ventilator’s expiratory port.
The Proof
The Pall Ulitipor100 filter has been validated to retain >99.999% of bacteria and viruses from monodispersed aerosols at the patient end of the breathing circuit. In a study from an independent laboratory, it was found to have the highest performance among 104 filters tested.3 The Pall Ultipor 50 filter stops monodispersed aerosols of bacteria at >99.999% and viruses at >99.995% efficiency at the ventilator’s expiratory port.
Both the Ultipor 100 and Ultipor 50 BCF have been validated for the retention of the SARS-CoV2 virus (registered for products under CE-mark, not in the USA).4,5
Our Products
The safety of patients and healthcare workers is our top priority. To prevent bacterial or viral contamination between patients and breathing systems, we’ve designed a range of high efficiency ventilation and breathing system filters. Get quality filters for anesthesia, intensive care and surgical gas handling.

Anaesthesia patient side
Our UltiporTM 25 Breathing Circuit Filter for anesthesia with high efficiency pleated hydrophobic membrane, provides an effective barrier against viruses, bacteria, and liquid-borne contaminants.

Anaesthesia circuits and kits
(Only available with FDA clearance)
Our multi-patient-use breathing circuits can be used between patients for up to 24 hours if every patient is provided with a new Pall UltiporTM 25 breathing circuit filter. This set up is protecting patients, staff, and equipment while increasing efficiency and reducing costs.

Anesthesia and ICU patient side
Our UlitporTM 100 Breathing Circuit Ffilter with high efficiency pleated hydrophobic membrane, provides an effective barrier against viruses, bacteria and liquid-borne contaminants, and ensures physiological humidification of breathing gases. It can also be used for drug nebulization between the filter and the patient.
If no nebulization is used, the service life of UltiporTM 100 can be extended from 24 to 48 hours.

Machine and patient side anesthesia
Our UltiporTM 50 & 55 Breathing Circuit Filter with highly efficient pleated hydrophobic filter medium is designed for ventilator machine side applications and provides an effective barrier for viruses, bacteria, and liquid-borne contaminant. It can also be used as a heat and moisture exchanger filter at patient end in anaesthesia applications.

Highly efficient surgical smoke evacuation
Our LaparoShield® Laparoscopic Smoke Filtration System with ULPA filtration rating and Viral and Bacterial retention, delivers protection for healthcare workers and patients exposed to surgical plume. It is easy to use and works without the need for external pumping equipment.
Insufflation Gas Filtration
Protect your equipment with our IGF1 Insufflator Gas Line Filter (CE Mark) high efficiency hydrophobic filter medium, protecting against microorganism, particles and backflow of bodily fluids and blood.
References
Hallgren F. et al. (2021). Particle flow rate from the airways as fingerprint diagnostics in mechanical ventilation in the intensive care unit: a randomised controlled study. ERJ Open Res; 7
Ari A. et al. (2016). Secondhand aerosol exposure during mechanical ventilation with and without expiratory filters: An in-vitro study. Ind J Resp Care; 5(1): 677-82
Wilkes A.R. (2004). Breathing System Filters. MHRA Evaluation Report 04005.
Spiers S. & Quarti C. (2021). Filtration Efficiency of the Pall Ultipor® 100 for SARS-CoV-2. Pall SLS Technical Report.
Spiers S, Quarti C. (2021). Filtration Efficiency of the Pall Ultipor® 25 for SARS-CoV-2. Pall SLS Technical Report.
The products advertised within this website may not have been licensed in accordance with local regulatory laws. Please check with the local Pall office for availability.